The menstrual cycle starts during puberty, and its onset is known as menarche. The age at which this occurs varies from woman to woman, but currently the average age is around 12 years old. When your periods start for the first time it is not unusual for your cycle to be erratic, and it can take several years for this to settle down and a regular cycle to be established.
The menstrual cycle finishes at the time of menopause. This is associated with a reduction in hormones being produced, most notably oestrogen. This causes your monthly cycle to cease, and your periods to eventually stop altogether. This marks the end of your fertility and ability to have children. Currently the average age of menopause is 51 years, although there is a condition called premature ovarian failure which causes this to happen earlier.
Menstrual Cycle Length
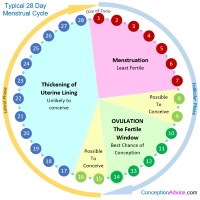
The normal menstrual cycle ranges from 21 – 35 days, but varies from woman to woman. Only 15% of women will have the “classical” 28-day cycle.
Shorter (< 21 days) or longer (> 35 days) cycles may indicate that ovulation is not happening. Not all cycles will result in ovulation, but if your cycle is consistently outside of this range, it may be worth discussing this with your doctor.
The variability in cycle length is usually related to variability within the initial part of the cycle, known as the follicular phase. Once ovulation occurs, the length of the second half of the cycle, the luteal phase, is fairly fixed at around 14 days. Therefore, in a regular cycle, ovulation can be predicted as occurring 14 days prior to the first day of the next due period.
Menstrual Cycle Phases
The menstrual cycle can be roughly divided into two different phases:
- Follicular Phase – the first half of the cycle including the period
- Luteal Phase – the second half of the cycle once ovulation has occurred
For explanation purposes, I will discuss these two different phases in more depth, as well as discussing the period and the time of ovulation. To make it easier to understand, I will assume that the cycle length is 28 days.
The Period
This refers to the bleeding that occurs at the beginning of the menstrual cycle. The first day of proper bleeding (as opposed to spotting that some women experience at the beginning of the period) is known as “Day 1” of your cycle.
The bleeding is caused by the shedding of the lining of the uterus – known as the endometrium. It is this lining which is important for the implantation of a fertilised egg, and if pregnancy has not occurred, then it is lost through the period each month at the start of the cycle.
Bleeding can last varying amounts of time, but usually is around 3-5 days in length. It may be associated with cramping pelvic pains. The heaviness of the flow of blood also varies from woman to woman, with some women only having light bleeding and others experiencing clots and flooding. The heaviness of the period and the degree of pain does not directly correlate with your fertility potential, but if you have extreme symptoms, such that they require you to miss work and spend days in bed, it may be an indication of a condition called endometriosis and you may wish to see your doctor to discuss your symptoms further.
The Follicular Phase
This is the first half of the cycle. In an average 28-day cycle, this would last from day 1 of the cycle through to day 14. The most important aspect of this stage is the development of the egg within the ovary ready for ovulation.
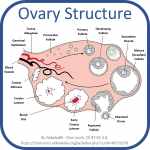
At the start of the cycle, there are multiple different follicles in the ovary which are ready to start maturing to be possibly ovulated during that cycle. A follicle is a small pouch like structure within the ovary which contains an egg. There are hundreds of thousands of these within each ovary, but it is only usually one which matures sufficiently to be ovulated each month. The full maturation process takes around 3 months, so there is always a group of developing eggs being prepared at any time. These are known as antral, or resting, follicles, and assessing the number and size of these by ultrasound scan can be helpful to determine your fertility potential and ovarian reserve. This is done through an antral follicle scan.
During the follicular phase, under the influence of the hormone aptly called Follicle Stimulating Hormone (FSH), a small number of resting follicles make the jump and start to mature. At around days 5-7 of the cycle, one of these maturing follicles will become “dominant”. This dominant follicle then prevents the development of the other follicles, and becomes the follicle from which the egg will be ovulated when ready.
Under the influence of ovarian stimulating medications, such as those used during IVF treatment, it is possible to produce multiple “dominant” follicles. This is the process by which multiple eggs can be collected during the IVF cycle to maximise the chances of success.
Ovulation
Ovulation occurs on day 14 of a 28-day cycle. This is when the follicle, having fully matured, breaks open to release the egg. The egg then slowly progresses towards the fallopian tube, where the cilia (little hair like projections which line the tube), gently waft to and fro and encourage the egg to enter the tube. It is here that the egg would meet the sperm for fertilisation to occur.
The Luteal Phase
The luteal phase refers to the second part of the cycle, following ovulation and ending with the beginning of the period (should pregnancy not occur).
Once ovulation has occurred, the hormone levels change further. The follicle which burst open to release the egg becomes known as the corpus luteum (hence why this half of the cycle is called the luteal phase). This produces progesterone, which encourages the endometrium (the lining of the uterus) to become thicker and ready for implantation of the fertilised egg. If pregnancy does not occur, then this corpus luteum gradually shrinks away at the end of the cycle to allow the ovary to start follicle maturation again.
After 14 days, if there is no pregnancy, then the period starts with the shedding of the thickened endometrium, and the menstrual cycle starts all over again.
Menstrual Cycle Hormones
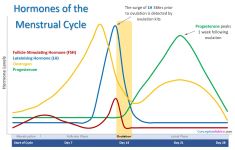
(Click to Enlarge)
Deep breath, here we go…
Follicular Phase
During the follicular phase, the main hormone is the Follicle Stimulating Hormone (FSH). This encourages the resting follicles to start developing and maturing, ready for ovulation this cycle. FSH is a gonadotrophin hormone, which means that it is a hormone released from the pituitary gland in the brain. Another hormone released from here at the same time is the Luteinizing Hormone (LH). These both act upon the developing follicles to help them mature, however at the start of the cycle the levels of FSH are much higher than those of LH. As the follicles are maturing they are producing oestrogen.
The selection of the dominant follicle is the result of a complex feedback of hormones between the ovary and the pituitary gland. As the dominant follicle tends to be the biggest and most developed of the follicles, it requires less FSH than the others in order to develop further. This is important as the levels of circulating FSH starts to drop around the mid-follicular phase (roughly day 7 of the cycle). This decline prevents the smaller follicles from developing further, but allows the dominant follicle to continue growing until it is fully mature. When these levels of FSH don’t decline (as occurs during ovarian stimulation during an IVF cycle), multiple dominant follicles develop ready for egg collection.
The developing follicle produces oestrogen. When the oestrogen reaches a sufficient level, it encourages the pituitary gland to release more LH. This causes an initial gradual rise in circulating levels of LH from around day 8 to day 12 of the cycle. The LH levels increase more rapidly from day 12 onwards. This rise allows the follicle to prepare for ovulation, and also causes the progesterone levels to start to rise slightly. This production of progesterone causes a “surge” in LH levels. Around 36 hours following this surge, ovulation occurs. It is this increase in LH which ovulation kits are trying to detect.
Luteal Phase
After ovulation, the corpus luteum forms from the ruptured follicle. This produces progesterone, which is responsible for the increase in your basal body temperature that is seen after ovulation. This suppresses the pituitary gland and prevents it from releasing high levels of FSH and LH.
This phase lasts for around 14 days, and towards the end the corpus luteum starts to disappear, if pregnancy has not occurred. This results in lower levels of circulating progesterone and oestrogen, which allows for the levels of FSH and LH to start rising again at the start of the new cycle. It also causes the endometrium to die and be shed, and menstruation to start.
If fertilisation of the egg and implantation has occurred, the progesterone levels do not fall. The developing embryo releases progesterone, which prevents the rise of FSH and LH, and prevents the shedding of the endometrium and your period starting.
Menstrual Cycle Symptoms
The most obvious symptom of your whereabouts in your menstrual cycle is your period. Unfortunately, after this, it can get a bit difficult to determine where you are in your menstrual cycle. If you have a cycle that is regular as clockwork, then this is easier, as ovulation is likely to occur on roughly the same day each cycle. However, most women’s cycles are not that regular that they can rely on counting alone.
The reason why it is helpful to know where you are in your menstrual cycle is when you are trying to conceive. There is only a short time window where you can get pregnant each cycle – as the egg only survives for 24 hours following ovulation. Therefore, recognising when ovulation is occurring may well reduce the time it takes for you to get pregnant. The hormonal changes that occur during the menstrual cycle, make other changes in your body which can be identified as a sign that ovulation is about to happen, or has happened recently. These signs include changes in basal body temperature, changes in cervical mucus and in cervical position. These are all large topics in their own right, so for more information check out: Ovulation Signs and Symptoms
Long Follicular Phase
The typical follicular phase lasts on average between 13 – 15 days. It is not uncommon for women who have long cycles to have longer follicular phases in comparison to the length of their luteal phase. This is not necessarily a problem. Sometimes a longer follicular phase might indicate that a dominant follicle is taking a while to develop and this may be an indication of reduced egg quality. However, this sign alone is not sufficient to make that diagnosis, and you would need to have the corresponding hormone changes found by blood tests to confirm this. It is more likely that you have either always had a slightly longer follicular phase, or that the follicular phase length has been altered by environmental changes around you – such as stress, changes in weight or exercise. These factors can either speed up or delay ovulation, thus affecting the length of your follicular phase.
Shortened Follicular Phase
As women become older their follicular phase tends to shorten. This again is not necessarily a problem, although if it is too short, the dominant follicle may not have had a sufficient chance to mature. There is no specific length cut-off for this diagnosis, and again you would need further investigations to determine whether or not a shortened follicular phase is a sign of other fertility problems.
Long Luteal Phase
The luteal phase is usually between 11 – 14 days in length, and therefore anything longer than this is deemed a long luteal phase. Again, this is not usually a problem as it is not thought to interfere with fertility and becoming pregnant. It will mean though that your cycles are likely to be longer than the typical 28 days.
Shortened Luteal Phase
A shortened luteal phase is one which is shorter than 11 days in length. This can be a problem if you are trying to conceive as if it is shorter than the usual 2 weeks, the endometrium has not had sufficient time to thicken and allow for implantation. It is very difficult to diagnose a shortened luteal phase accurately yourself, and if you are concerned that this may be happening to you I would advise speaking to your doctor. Having a short cycle length does not automatically mean that your luteal phase is shorter than needed to establish pregnancy.
This is not a common condition, and is usually corrected by improving lifestyle factors especially diet, to ensure that you are consuming sufficient vitamins and minerals, and ensuring that you are not underweight. If this does not improve the length of the luteal phase then sometimes medications such as progesterone or Clomid may be beneficial.
Menstrual Cycle Calendar
I strongly advise every woman, regardless of whether or not they are trying to conceive, to keep track of their menstrual cycle. Consistent changes within a woman’s typical menstrual cycle may indicate that there is an underlying problem – for example regular bleeding in between periods may be a sign of an infection.
When trying to conceive, keeping track of your cycle becomes even more important. It can help you to identify when is the most fertile time of the month for you, and hence how you can maximise your chances of conceiving. This can be done just by keeping a track of when your last period arrived and so being aware of when your next period is due. Alternatively, you can look in real depth at your cycle and body’s response to the changes in hormones throughout the month through a process called charting. This can be a more accurate way of determining when ovulation is occurring for you, and may even help you to detect the very early signs of pregnancy even before a pregnancy test!
Links to Popular Related Pages